COVID-19 VACCINE & TESTING INFORMATION AND RESOURCES
UPDATE 4/1/23:
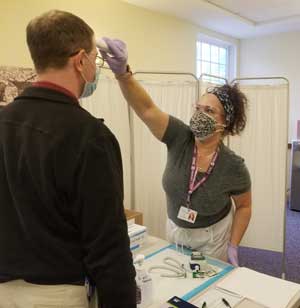
Masking is now optional in all DMC clinics unless any or all of the following circumstances are present at time of visit:
- The patient/child has been recently exposed to the COVID-19 virus
- The patient/child has tested positive for the COVID-19 virus within the past 10 days
- The patient/child is experiencing upper respiratory symptoms.
UPDATE 9/10/22:
DMC has the latest COVID-19 booster (Bivalent) available in our offices. Please call 603-537-1300 to
schedule a visit for your booster.
COVID-19 Vaccination/Booster Details:
- As of 9/10/22, we have Pfizer and Moderna Bivalent boosters available. Patients 12 and older who have received their primary vaccine doses (or a single dose of J & J and are 18 and older) are eligible. You may have received other boosters as well but should wait at least 2 months before getting the Bivalent booster.
- Patients 5 – 11 years who have completed their primary vaccine doses can receive a booster (Monovalent).
- We have primary doses of Moderna and Pfizer for patients 6 months and older who have not received them.
- If you have received a primary or booster dose of any vaccine, the CDC recommends waiting at least two months before getting a Bivalent booster. Please talk with a DMC representative about any vaccines you have already received when you make your appointment.
- The CDC recommends waiting a minimum of two months after contracting the COVID-19 virus to get any booster.
- If you are an immunocompromised individual, please let your DMC representative know when you make your appointment.
- If you are receiving a COVID-19 vaccination or booster and have received at least one dose prior to your appointment, please be sure to bring your vaccination card to your appointment.
UPDATE 3/21/22:
DMC has moved all COVID-19 testing and vaccines into our clinics. If you need testing or would like to be vaccinated, please call our main number at 603-537-1300 and let the patient service representative know which office location is most convenient for you.
UPDATE 2/11/22:
Effective February 11, 2022, DMC is once again able to expand COVID-19 testing to include patients who are not experiencing symptoms. Asymptomatic patients who need testing to return to work or school, for travel, social events or pre-surgery can call our main phone number 603-537-1300 to make an appointment for our drive-through clinic at 15 Tsienneto Road in Derry. Testing for patients who are experiencing symptoms will continue at the drive-through as usual, also by appointment.
UPDATE 1/31/22:
- COVID-19 Vaccines In-Office: You can request a vaccine at any regular office visit or you can call to schedule a short “Nurse Visit” appointment to get your vaccine. Please be sure to bring your vaccine card if this is not your first COVID-19 shot. Appointments are required.
- COVID-19 Vaccines at DMC Drive-thru Clinic: Please call to make an appointment for the DMC Drive-through Clinic. Please bring your vaccination card if this is not your first COVID-19 shot.
-
- 12 years and older: Wednesdays from 9:00 am-11:00 am at 15 Tsienneto Road, Derry
- 5-11 years old: Saturdays Only from 9:00 am -11:30 am at 15 Tsienneto Road, Derry
- COVID-19 Testing for SYMPTOMATIC Patients Only via DMC Drive-through Clinic at 15 Tsienneto Road, Derry. Appointments are required.
- Mondays, Tuesdays, Thursdays and Fridays: 9:00 am -11:00 am & 1:30 pm -3:30 pm
- Wednesdays: 1:00 pm -4:00 pm
UPDATE 1/14/22
COVID-19 TESTING AT DMC CURRENTLY FOR SYMPTOMATIC PATIENTS ONLY
DMC remains committed to providing COVID-19 testing for our patients who are experiencing illness and symptoms, especially those at high risk for developing complications, or who are immune-compromised. However, due to very high demand, DMC is not able to provide COVID-19 testing for asymptomatic patients (patients who do not have symptoms) until further notice. It’s also important to note that antigen (rapid) tests are not as reliable in asymptomatic patients and PCR tests currently have a turnaround time that is typically not helpful for asymptomatic patients who need results for travel, surgery, etc. Patients who are not experiencing symptoms but want or need to be tested, do have other resources available.
1. Vault (PCR testing program through the State of NH)
- This is an at-home PCR testing program
- Testing kits are available direct-to-consumer and available at community distribution points (Schools, FQHCs, homeless shelters, municipalities, PHNs)
- Testing kits will be mailed directly to the individual
- Results are available within 48 hours of being received in the laboratory
- An individual is eligible to order another test once the lab results are available
- Testing is free
Vault COVID-19 Testing: No-Cost COVID Testing for All Areas of New Hampshire (vaulthealth.com)
2. COVID-19 Fixed Testing Sites (through the State of NH)
There are currently four fixed testing sites in NH (Nashua, Manchester, Newington, and Claremont). These are scheduled to remain operational until 3/31/2022. There are four new sites slated to open in January (locations TBD).
- Appointments are NOT required for any of these sites
- Sites will test both asymptomatic and symptomatic individuals
- Testing is free
- Turnaround time is currently 72 hours
State of NH Fixed Site Testing: https://ccmdcenters.com/state-of-nh-covid-19-testing
3. Say Yes Covid Test (Quidell antigen testing program)
- This is an at-home antigen testing program
- Testing supplies are available direct-to-consumer (delivered to individual homes) and available at community distribution points (Schools, FQHCs, homeless shelters)
- These tests are available while supplies last
- Anyone who ordered these tests for the first phase of this program is not eligible to receive additional tests during this phase
- Each order will be provided with 4 tests (2 boxes)
Say Yes! To Covid Test: https://sayyescovidhometest.org/
4. Labcorp COVID-19 Testing Options
If you are symptom-free and have had no known exposure, Labcorp offers in-person testing at select Labcorp locations for travel, event, or gatherings. You do not need an order from a DMC physician but you do need to reserve or purchase your kit online before arriving in person. These in-person tests are for asymptomatic patients who have not been exposed. Online appointments are encouraged. Labcorp is are also currently taking a limited number of orders for COVID-19 home collection kits. There may be a fee associated with these tests.
Labcorp On Demand: https://www.ondemand.labcorp.com/covid-19-pcr-tests
IMPORTANT NOTE: Individuals with severe symptoms such as difficulty breathing or chest pains should access emergency services. If you do not have symptoms but wish to be tested for COVID-19, please consider the options above before going to an ER. A hospital emergency room visit should be reserved for life threatening conditions.
UPDATE 12/22/21
DMC has added more days and times to our COVID-19 Vaccination Drive Up.
From Monday 12/27 through Friday 1/28 (Dose #1, #2, or Booster):
- For 12 years and older: Monday – Friday 9:00 am to 11:30 am (Pfizer, Moderna, J&J)
- For 5 – 11 years old: Saturdays 9:00 am to 11:30 am (Pfizer)
COVID-19 Drive Up Testing will continue to be offered Monday – Friday from 1:00 pm – 4:00 pm.
PLEASE NOTE THAT ALL VACCINATIONS AND TESTING REQUIRE AN APPOINTMENT. PLEASE CALL 603-537-1300.
UPDATE 12/1/21
The State of NH has announced that there are 10,000 COVID-19 booster shots available to adults 18+ at locations throughout the state. To learn more or to find the closest booster site, please click HERE .
UPDATE 11/05/21
DMC DRIVE UP PEDIATRIC COVID-19 VACCINATION CLINICS
• Pediatric COVID-19 vaccines are available for 5-11 year olds via our Derry Drive Up location starting Saturday, November 13th from 1:00 pm to 3:00 pm.
•Saturday clinics will be held on November 20th, December 4th and December 11th from 8:00 am to 11:30 at our Derry Drive Up location.
• APPOINTMENTS ARE REQUIRED. Please call 603-537-1300 to schedule or use the Contact Us form on our website (CLICK HERE) to request an appointment for your child’s COVID-19 vaccine shot.
• All Saturday Drive Up Clinics are held at 15 Tsienneto Road, Derry, NH in the back of the building.
• A parent or legal guardian must be present for any child to receive vaccine.
UPDATE 10/7/21
DMC DRIVE UP COVID-19 VACCINATION AND TESTING SITE
- DMC is currently offering drive up COVID-19 vaccinations by appointment only on Mondays, Wednesdays and Fridays from 9:00 am to 11:00 am. PLEASE NOTE: IF YOU WILL BE RECEIVING YOUR SECOND OR THIRD DOSE OF ANY COVID-19 VACCINE, YOU MUST BRING YOUR ORIGINAL VACCINATION CARD WITH YOU TO YOUR DRIVE UP APPOINTMENT. DMC’s drive up site is for DMC patients only and the schedule is subject to change.
- DMC is currently offering drive up COVID-19 testing by appointment only Monday through Friday from 1:00 pm to 3:30 pm. COVID-19 testing is for DMC patients only and the schedule is subject to change.
UPDATE 9/16/21
DMC COVID-19 VACCINE EXEMPTION LETTER POLICY
DMC has recently received phone calls from patients requesting a medical exemption letter for the COVID-19 vaccine. As some employers, schools, and other organizations have started to require individuals to become fully vaccinated, we at DMC wanted our patients to know our policy on this matter.
DMC will follow CDC guidelines to assist patients who qualify for a medical exemption, however, only a very small percent of our patient population meets these criteria. DMC is not able to provide a letter of medical exemption to patients who do not meet CDC criteria.
In order to secure a medical exemption letter from DMC, a patient must have:
- Documented history of severe allergic reaction to a component of each currently available COVID-19 vaccine
OR
- Documented history of severe allergic reaction to a COVID-19 vaccine
OR
- Documentation of receiving antibodies for treatment or prophylaxis against COVID-19 in the past 90 days
OR
- Current treatment with certain immunosuppressive agents (In this case, the exemption letter must come from your prescribing specialist, not DMC)
If you feel that you qualify for a medical exemption based on the above criteria, you MUST schedule an appointment with a DMC provider for an in-office or virtual evaluation. If your provider determines that exemption is medically necessary (based on CDC criteria) an exemption letter will be provided to you.
Examples of conditions that the CDC does NOT consider a medical exemption include:
- History of COVID-19 infection or positive antibody screen
- History of severe allergic reactions to foods, latex, pets, insects, medications or environmental triggers
- Fear of needles
- History of vaccine side effects or general avoidance of vaccines
- Cancer, leukemia, HIV, or autoimmune disease
- Pregnancy (in any trimester) or contemplation of pregnancy
- Recent immunization with any other vaccine
- Personal or family history of Guillain Barre Syndrome
- Current or anticipated breast feeding
Thank you – we appreciate for your cooperation and support in this matter!
UPDATE: 8/16/21
On August 12, 2021, The CDC issued recommendations for a third dose of Pfizer and Moderna COVID-19 vaccines for certain people who are moderately to severely immunocompromised only. This is NOT a booster shot for the general public as the booster shot is still being developed.
DMC patients who qualify for a third dose will have:
- Been receiving active cancer treatment for tumors or cancers of the blood
- Received an organ transplant within the last two years or are taking medicine to suppress the immune system
- Moderate or severe primary immunodeficiency (DiGeorge Syndrome, Wiskott-Aldrich Syndrome)
- Advanced or untreated HIV infection
- Active treatment with high-dose corticosteroids or other drugs that may suppress your immune response
If you feel you may qualify for a third dose of either Pfizer or Moderna please contact DMC at 603-537-1300 to set up a virtual visit for evaluation by a provider. Upon evaluation you may be scheduled to receive your third dose.
UPDATE 6/2/21
DMC will begin offering DRIVE-UP vaccine appointments in Derry, starting Monday, June 7th. Appointments are necessary. Please call our main number at 603-537-1300 to schedule your COVID-19 immunization. We will be rotating Pfizer, Moderna and Johnson & Johnson vaccines. Children will only receive Pfizer.
- If you have multiple household members who need vaccination, please let us know when you call to book your appointment. We can vaccinate more than one individual in the same vehicle at the drive-up site.
- If this is your first dose of any COVID-19 vaccine, DMC will contact you to schedule your second dose within the appropriate window of time (if needed). However, if you do not hear from DMC within two weeks, please call us to schedule.
- DMC will provide patients with an immunization card stating the date of each dose and type of vaccine.
- If you received your first dose of any COVID-19 vaccine somewhere other than DMC, YOU MUST BRING YOUR VACCINATION CARD TO YOUR APPOINTMENT to ensure that your second dose is the same type as the first and that the timing between doses is appropriate.
- Required observation time following your immunization is 15 minutes (30 minutes if you have a history of reactions/allergies).
- If you are experiencing any symptoms of COVID-19 (cough, fever, shortness of breath, etc.) on the day of your scheduled immunization, please call the office to reschedule your vaccine appointment and receive COVID-19 evaluation/testing instead.
Update 5/10/21
DMC is no longer offering monoclonal antibody treatments. We are glad to have supported our community and to have helped many people with COVID-19 avoid severe symptoms and hospitalization.
Update 4/16/21
MASKS CONTINUE TO BE REQUIRED AT DMC
The State of New Hampshire announced that the mask mandate will be lifted effective today, Friday, April 16, 2021. PLEASE NOTE: This doesn’t mean the pandemic has ended. DMC will continue to observe masking protocols in all of our medical facilities. In order to protect our patients, staff, and caregivers masks are required until further notice. Thank you for your cooperation and support.
Update 4/1/21
Starting tomorrow, April 2nd, individuals age 16 and older are eligible to register for COVID-19 vaccination in the state of NH. (Due to FDA emergency use authorization requirements, recipients who are 16 and 17 years old may only receive the Pfizer vaccine.)You can click HERE to register for an appointment with the State to view COVID-19 data for NH.
Update 3/18/21
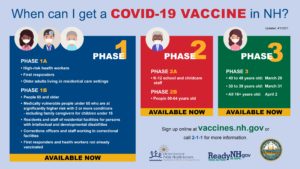
As New Hampshire’s vaccination effort remains ahead of schedule, appointments at state-managed fixed sites for Phase 2A will begin on Thursday, March 18.
All staff working in New Hampshire in the following settings are eligible for vaccination under Phase 2A:
• K-12 schools
• Licensed child care settings
• License-exempt settings enrolled with the NH DHHS – Bureau of Child Development
• Municipal or other recreation programs providing before and/or after school, vacation, or summer youth programming
• Head Start and Early Head Start Programs
• Licensed youth camps
Registration for individuals between 50 and 64 years of age will begin on Monday, March 22 at 8:00 AM under Phase 2B, with appointments beginning on Thursday, March 25.
The fastest way to schedule an appointment is through vaccines.nh.gov. An extremely high call volume to 2-1-1 is anticipated. Wait times may be long, but every call will be answered by a live person.
Update 2/17/21
Last week, the State of NH announced a partnership with pharmacy chain, Walgreens to assist vaccination efforts starting with Phase 1B. According to a story on WMUR.com:
“Anyone with a Walgreens appointment must meet current state guidelines for eligibility. The state is in Phase 1B of vaccinations, meaning anyone age 65 or older can be vaccinated, along with younger people with two or more comorbidities that raise their risk of serious illness.
State officials said they will be scheduling people for appointments at Walgreens, starting with those who have already booked the latest appointments. For example, someone who could previously only find an appointment in April would likely be among the first to get a call for an earlier appointment at a Walgreens.”
Read the story HERE.
DMC Launches Monoclonal Antibody Clinic 1/26/21
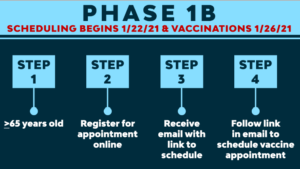
Important Update 1/22/21
Many patients received a message erroneously generated by State’s website instructing them to contact their primary care office for help scheduling their COVID-19 vaccine. The State is working to correct this glitch. DMC does not have access to vaccine registration or scheduling and cannot assist you in getting an appointment.
If you are 65+ you are automatically eligible to register during Phase 1B (which starts today). We urge you to go ahead and register online or by calling 2-1-1.
If you are 64 or under and qualify for Phase 1B due to medical conditions, you should have received notification from DMC by email or phone, that we have already provided your confirmation to NH DHHS. The State is processing this information and will be contacting you directly in the next week or so. No further action is necessary at this time. Those 64 and under who qualify due to medical conditions will not be able to complete their registration online for the vaccine until they are contacted by the State. We understand that you may be anxious to register for the vaccine. We have been told that our patients’ info has been received by the State and they are working to start outreach today. It may be several days to a week before you hear from the State. Please know that DMC has followed all instructions that we received from the State in order to help you. Please be patient.
Once you have successfully registered, you will receive further instructions from the State to set up your vaccine appointment. The State has advised that appointments may be several weeks out.
Please reach out to the State directly with vaccine-related questions by dialing 2-1-1.
January 15, 2021
At DMC Primary Care, plans are underway for the next wave of vaccinations in our fight against COVID-19, and we will continue to update you so that you know what to expect.
Beginning on Friday, January 22nd, our patients who are 65 years or older will be eligible to register for the COVID-19 vaccine at www.vaccines.nh.gov as part of Phase 1B in the State’s vaccine rollout plan. You will be able to select your appointment location, date and time. We encourage DMC patients 65 and over who live in NH to consider registering. You do not need a doctor’s order to register for your vaccine shot. Simply provide proof of age at your appointment at one of the State’s vaccine sites.
Another group of NH patients that will be eligible under the New Hampshire’s vaccine plan are individuals that are considered medically vulnerable (defined by the CDC as having two or more of the medical conditions at higher risk for developing severe symptoms from COVID-19). DMC Primary Care has reviewed the medical records of our patients and identified those individuals that meet the State’s guidelines. We are in the process of notifying our patients who are eligible by telephone or email. This notification will be completed prior to 1/22/21.
We have already submitted information to NH DHHS for our patients who meet the guidelines for medical vulnerability. It is important for you to know that DMC did not disclose any information on specific medical conditions that our patients have (no Personal Health Information – or PHI – was shared). Beginning on Friday, January 22, the State will start contacting our medically vulnerable patients directly with information on how to schedule their vaccine appointment.
This does not mean that you consent to receive the vaccine. We do recommend the vaccine for all patients who are at high risk of developing severe symptoms from COVID-19, however, it is your choice whether to register to receive the vaccine or not.
Please do not contact the office for confirmation of medical vulnerability.
For COVID-19 vaccination questions, please contact the State of NH by dialing 211.
DMC is not administering vaccines, so please do not contact your provider for vaccination information. We will post any vaccine updates to this page as they occur. Please check back often.